Abstract
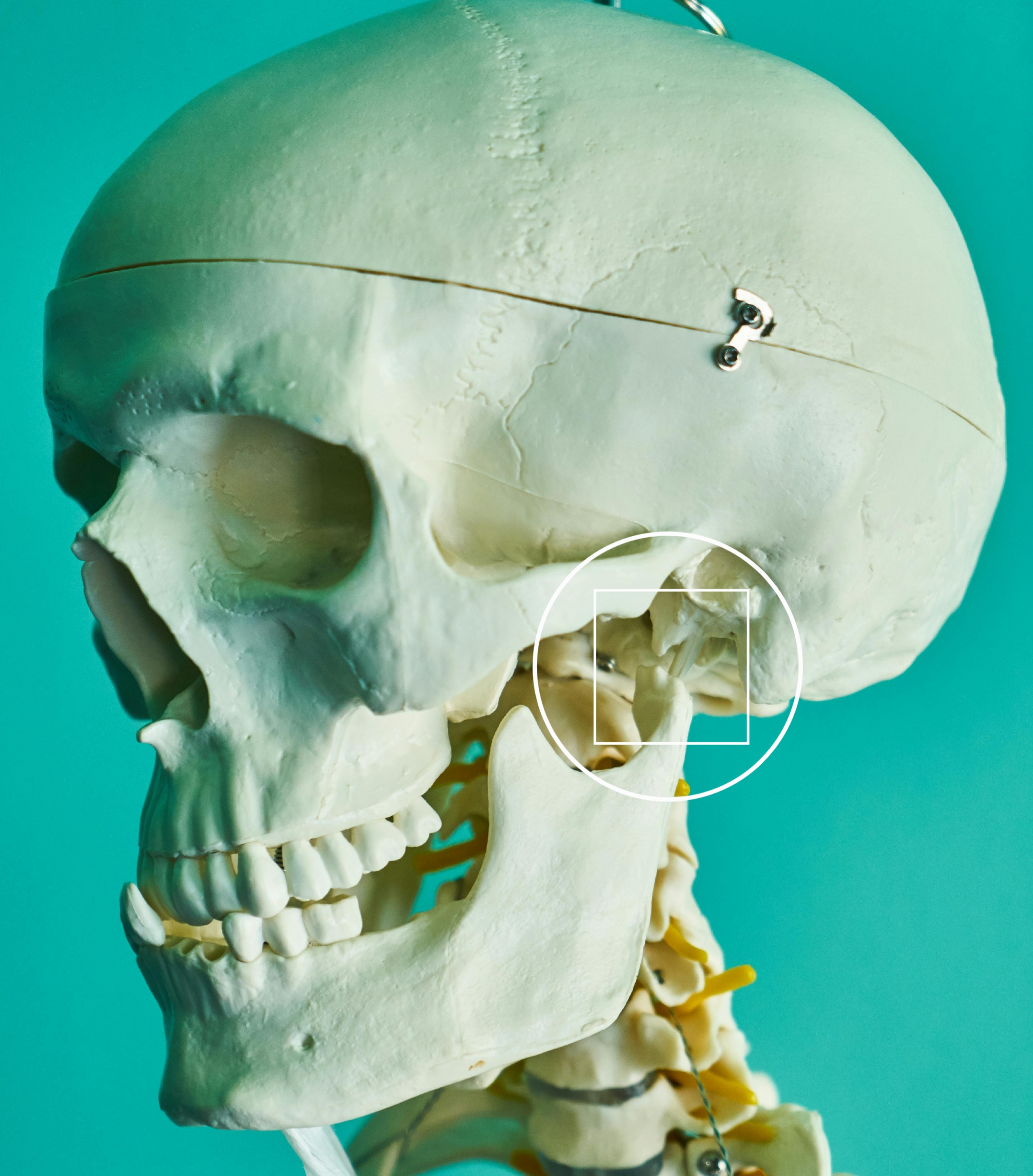
Temporomandibular disorders (TMD) encompass a range of conditions affecting the temporomandibular joint (TMJ) and associated musculoskeletal structures, often leading to pain and functional limitations. Occlusal rearrangement treatments, including occlusal adjustments and splint therapies, are commonly employed to alleviate TMD symptoms. This article reviews the recurrence rates of TMD following such interventions, drawing on current scientific literature.
Introduction
TMD affects a significant portion of the population, presenting with symptoms such as jaw pain, restricted movement, and joint noises. Occlusal rearrangement treatments aim to modify the contact and alignment of teeth to reduce these symptoms. Understanding the long-term efficacy of these treatments, particularly concerning symptom recurrence, is crucial for clinical decision-making.
Occlusal Rearrangement Treatments
Occlusal interventions include occlusal adjustments (selective grinding of teeth to improve occlusal harmony) and occlusal splints (devices designed to alter the occlusal relationship temporarily). These treatments intend to reduce abnormal muscle activity and joint loading associated with TMD.
Recurrence Rates Post-Treatment
The recurrence of TMD symptoms after occlusal treatments varies across studies. A Cochrane review by Singh et al. (2024) analyzed 57 randomized controlled trials involving 2,846 participants and found insufficient evidence to conclusively determine the effectiveness of occlusal interventions in managing TMD symptoms. Notably, none of the included studies reported on discomfort or recurrence rates, highlighting a significant gap in the literature.
Another study observed that patients undergoing single-stage treatment with occlusal splints may experience a relapse of symptoms post-treatment, suggesting potential limitations in the long-term efficacy of such interventions.
Additionally, a long-term follow-up study reported that previously documented recurrence rates of TMD symptoms after conservative therapy were approximately 17.2%.
Discussion
The variability in reported recurrence rates may be attributed to differences in study design, patient populations, diagnostic criteria, and treatment modalities. The lack of standardized outcome measures further complicates direct comparisons across studies. Moreover, the absence of data on recurrence rates in many studies underscores the need for comprehensive long-term evaluations of occlusal treatments for TMD.
Conclusion
Current evidence regarding the recurrence of TMD symptoms following occlusal rearrangement treatments is inconclusive. The paucity of data on long-term outcomes, particularly recurrence rates, emphasizes the necessity for well-designed studies with extended follow-up periods to inform clinical practice effectively.
References
Singh, B. P., Singh, N., Jayaraman, S., Kirubakaran, R., Joseph, S., Muthu, M. S., Jivanani, H., & Hua, F. (2024). Occlusal interventions for managing temporomandibular disorders. Cochrane Database of Systematic Reviews, 2024(8), CD012850.
Skeletal, dentoalveolar and soft tissue changes after stabilization splint treatment in patients with temporomandibular disorders: A prospective study. (2024). BMC Oral Health.
Long-term follow-up of clinical symptoms in TMD patients who received conservative treatment. (2000). European Journal of Orthodontics, 22(1), 61-67.







Leave a Reply