

Introduction: Temporomandibular Joint Disorders and the Need for a National Framework
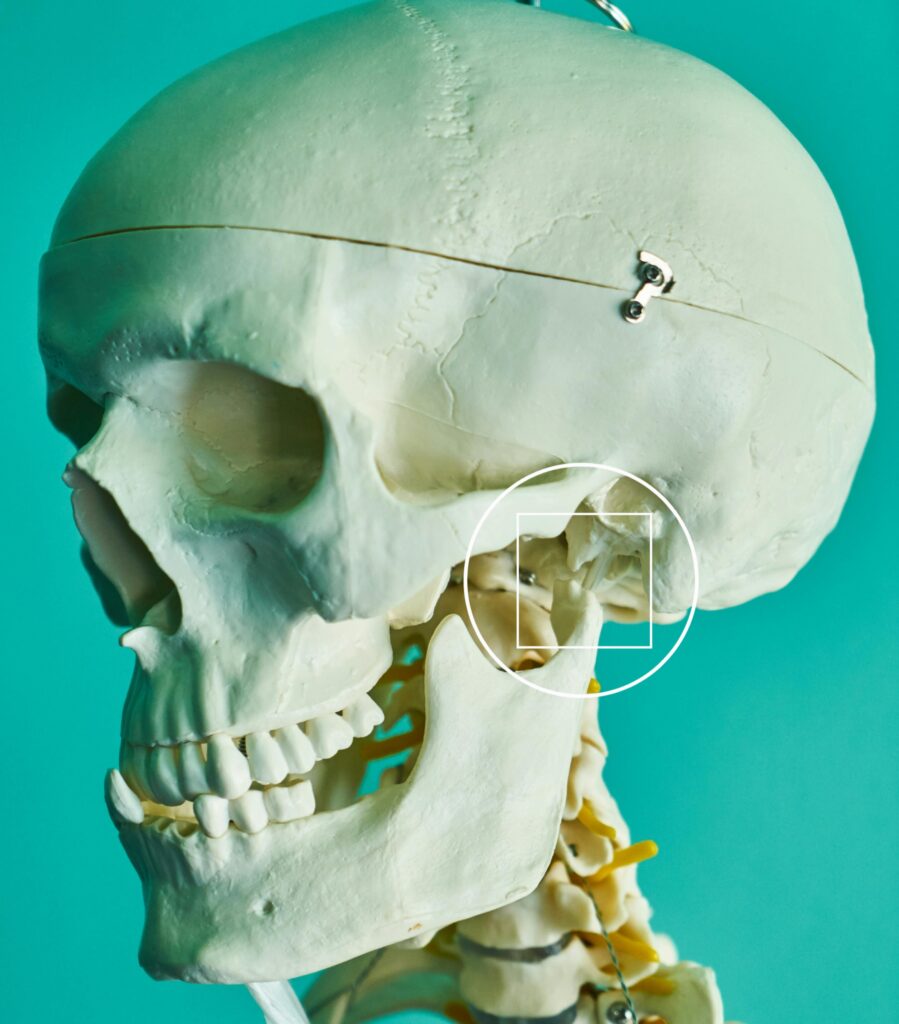
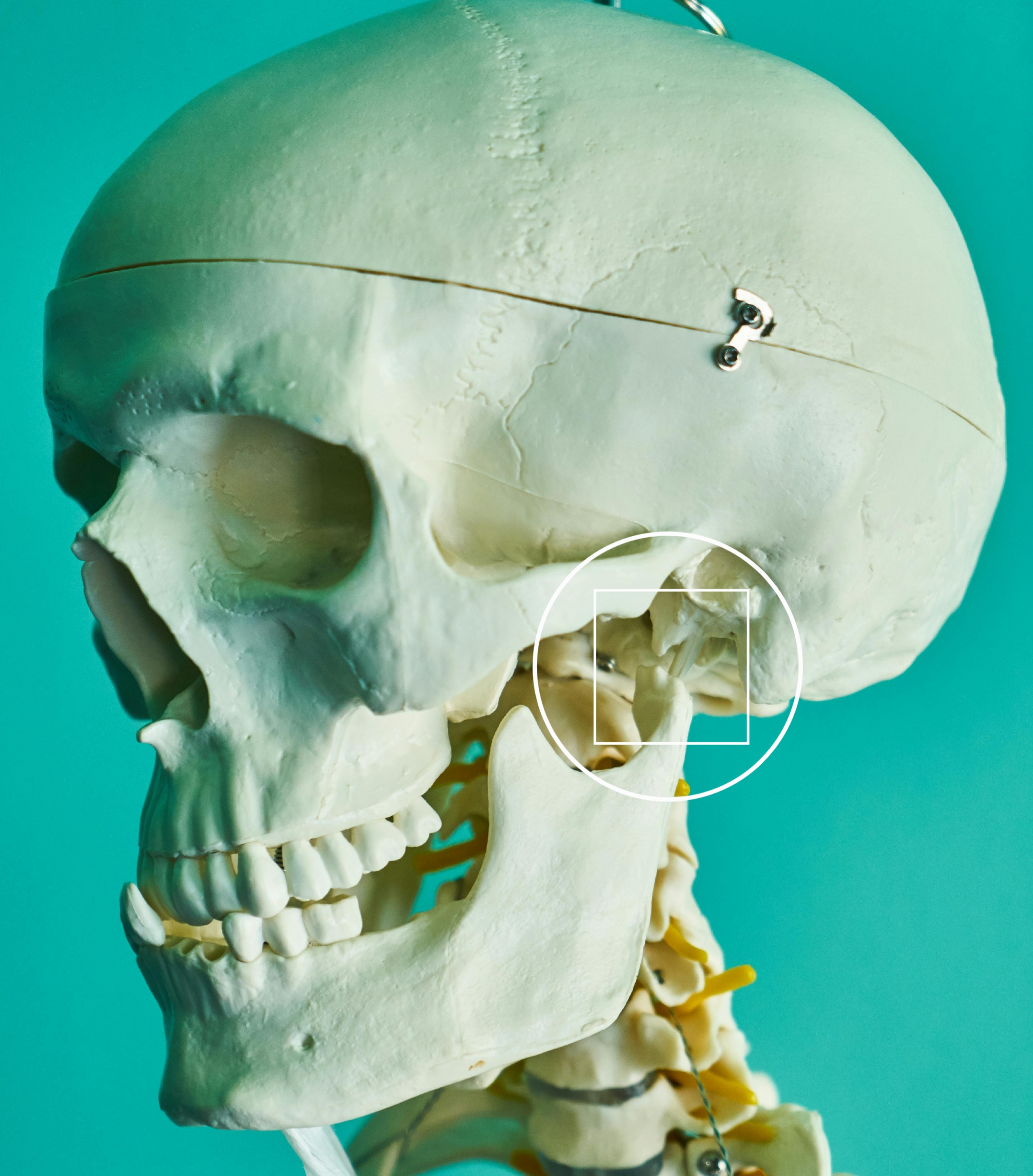
Temporomandibular Joint Disorders (TMDs) encompass a group of conditions affecting the temporomandibular joint (TMJ), masticatory muscles, and associated structures, leading to chronic pain, functional limitations, and reduced quality of life. Despite the high prevalence of TMDs—affecting up to 10–15% of adults and adolescents—there has historically been a fragmented and inconsistent approach to diagnosis, treatment, and research (National Academies of Sciences, Engineering, and Medicine [NASEM], 2020).
Due to increasing concerns about misdiagnoses, ineffective treatments, overreliance on irreversible interventions, and patient suffering, the U.S. Congress directed the National Institutes of Health (NIH) to commission the National Academies of Sciences, Engineering, and Medicine (NASEM) to evaluate the current landscape and provide comprehensive, evidence-based recommendations.
Why NASEM Was Tasked: Historical Context and Credibility
The National Academies of Sciences, Engineering, and Medicine is a private, nonprofit institution that provides independent, objective analysis and advice to the United States on complex scientific and policy matters. NASEM has a long-standing reputation for credibility, rigorous methodology, and multidisciplinary expertise. Since its founding in 1863, it has advised U.S. Presidents, Congress, and global bodies on critical health and scientific issues (NASEM, 2020).
The NIH and other federal agencies entrusted NASEM with this project due to its established framework for evidence-based, multidisciplinary, and patient-centered assessments. The TMD report was especially crucial given decades of controversy and the marginalized state of TMD care in mainstream medical and dental systems.
Methodology of the NASEM TMD Project
To undertake this project, NASEM convened a multidisciplinary committee consisting of experts in orofacial pain, dentistry, neurology, pain medicine, public health, psychiatry, and patient advocacy. The committee conducted:
- Systematic reviews of scientific literature.
- Public workshops with testimony from TMD patients, caregivers, clinicians, and researchers.
- Consultations with national and international experts in health policy, epidemiology, and clinical care.
- Evaluation of existing guidelines, research gaps, and clinical care standards across disciplines.
This methodologically rigorous approach culminated in the 2020 report titled “Temporomandibular Disorders: Priorities for Research and Care.”
Key NASEM Recommendations on TMD Management
- Multidisciplinary, Biopsychosocial Approach to Care
- TMDs should be recognized as complex, multifactorial disorders requiring integrated, multidisciplinary care incorporating physical, behavioral, and psychosocial therapies (NASEM, 2020).
- Establishment of Centers of Excellence
- Federal agencies should fund regional Centers of Excellence in TMD care and research, to serve as hubs for training, research, and comprehensive treatment (NASEM, 2020).
- Improved Education and Training in Dentistry and Medicine
- Dental and medical schools must integrate evidence-based TMD education, including pain management and interdisciplinary collaboration. Continuing education programs should address these critical gaps (NASEM, 2020).
- Patient-Centered Care Models
- Clinicians should engage in shared decision-making with patients and prioritize non-invasive, reversible treatments over irreversible interventions such as surgery or extensive prosthodontics unless strictly necessary.
- Enhanced Surveillance and Research Funding
- NIH and other agencies must prioritize TMDs in research portfolios, with longitudinal studies and data collection systems to better understand natural history, treatment outcomes, and risk factors.
- Interdisciplinary Research Collaborations
- Cross-institutional and interprofessional partnerships should be fostered to investigate the neurobiological, genetic, and environmental mechanisms of TMDs.
- Addressing Health Disparities and Access to Care
- Underserved populations should receive focused attention to reduce disparities in TMD diagnosis, management, and outcomes.

Significance for Philippine Dentistry: Education, Research, and Practice
The NASEM recommendations hold vital implications for the Philippines, where TMD care is also fragmented and underrepresented in both clinical and academic settings:
- Dental Education: Philippine dental schools often lack formalized, evidence-based training in orofacial pain and TMDs. Integrating NASEM’s curriculum recommendations can enhance clinician competence, reduce misdiagnoses, and improve interdisciplinary collaboration in the management of chronic orofacial pain.
- Clinical Practice: Many Filipino patients are subjected to irreversible treatments such as occlusal adjustments, orthotic devices, and unnecessary prosthodontic interventions. Adoption of NASEM-endorsed conservative, reversible therapies can improve patient outcomes and prevent harm.
- Research Development: There is a paucity of local data on the epidemiology, treatment outcomes, and biopsychosocial dimensions of TMDs in the Philippine context. By aligning with NASEM’s research agenda, Filipino institutions can contribute to global knowledge, secure international collaborations, and build national registries or Centers of Excellence.
- Public Health and Policy Advocacy: The interdisciplinary model endorsed by NASEM can inform Philippine health policies that recognize TMDs as chronic, disabling conditions requiring integrated care across dentistry, medicine, and allied health fields.
Conclusion
The NASEM report on Temporomandibular Disorders is a landmark document that redefines the clinical and research landscape of TMDs through a biopsychosocial lens. Its recommendations provide a scientifically grounded, patient-centered roadmap for reforming care delivery. For the Philippines, this presents an opportunity to modernize dental education, expand research frontiers, and elevate the standard of care for patients suffering from chronic orofacial pain.
References (APA 7th Edition)
National Academies of Sciences, Engineering, and Medicine. (2020). Temporomandibular disorders: Priorities for research and care. The National Academies Press. https://doi.org/10.17226/25652
National Research Council. (1863). An act to incorporate the National Academy of Sciences. https://www.nasonline.org/about-nas/legislation/nas-act-of-incorporation.html
U.S. Department of Health and Human Services. (2020). NIH’s role in the NASEM TMD study. National Institutes of Health. https://www.nih.gov/news-events/news-releases/nih-commissions-nasem-study-tmd-care
Interprofessional Education Collaborative. (2016). Core competencies for interprofessional collaborative practice: 2016 update. https://ipec.memberclicks.net/assets/2016-Update.pdf
Okeson, J. P. (2021). Management of temporomandibular disorders and occlusion (8th ed.). Elsevier.







Leave a Reply