by pinoydentalai
Abstract
Extraoral vacuum devices have emerged as effective tools for infection control, particularly in mitigating aerosolized particles during dental procedures. This review synthesizes evidence from recent studies to explore the efficacy, mechanisms, and clinical implications of extraoral vacuums. Research demonstrates their role in enhancing safety by reducing airborne contaminants, thus offering a supplementary measure in aerosol management alongside conventional protocols. Further investigation into device optimization and integration into diverse clinical environments is warranted.
Introduction
The COVID-19 pandemic highlighted the importance of robust infection control measures in healthcare settings, particularly in dentistry, where aerosol-generating procedures (AGPs) are routine. Aerosols generated during dental treatments pose risks of cross-contamination and disease transmission. Conventional measures such as personal protective equipment (PPE) and high-volume evacuators (HVE) have limitations, necessitating supplementary solutions. Extraoral vacuums (EOVs) have garnered attention for their potential to enhance infection control by capturing aerosols at the source. This article reviews recent advancements and clinical applications of EOVs, emphasizing their efficacy and integration into dental practices.
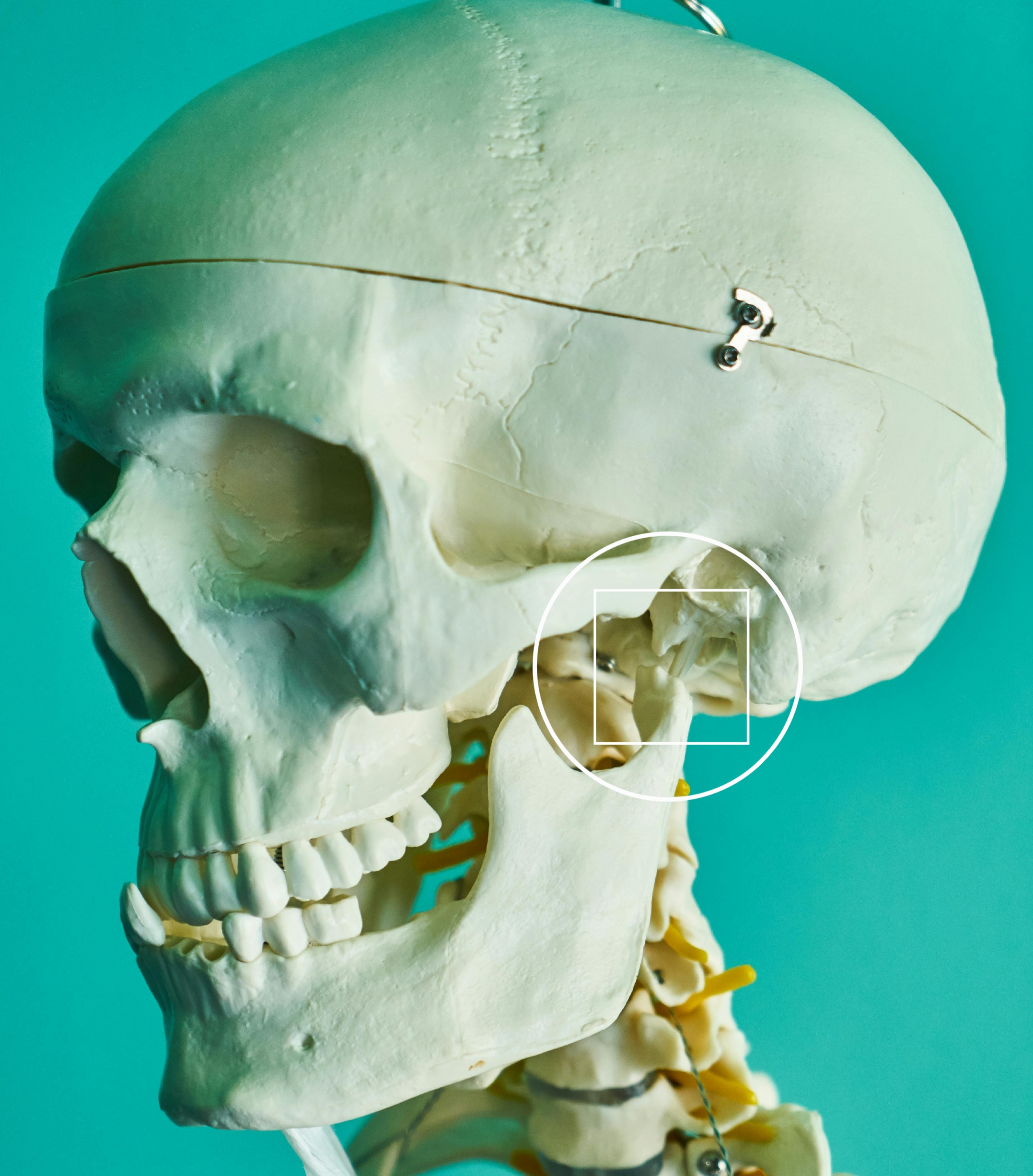
Mechanisms of Action
Extraoral vacuum systems function by positioning a high-powered suction device near the patient’s oral cavity to capture aerosols and droplets at the source. These devices typically combine filtration technologies, such as HEPA filters, with ultraviolet (UV) light or plasma sterilization to neutralize pathogens. Their efficiency depends on suction power, nozzle design, and placement proximity to the aerosol source. For instance, evidence shows that strategically placed EOVs can reduce aerosol dispersion by over 90%, significantly enhancing environmental safety【1】【3】.
Efficacy and Clinical Benefits
Aerosol and Pathogen Mitigation
Studies indicate that EOVs significantly reduce the concentration of airborne particles generated during AGPs. According to Gopalakrishnan et al. (2021)【1】, incorporating EOVs alongside HVE and rubber dams minimized aerosol dispersion by up to 99%. Similarly, Hashimoto et al. (2022)【3】reported the effective capture of bioaerosols, underscoring the role of EOVs in curbing potential exposure to infectious agents.
Patient and Practitioner Safety
The deployment of EOVs aligns with the goal of ensuring a safer clinical environment. By reducing aerosol density, these devices minimize the likelihood of inhalation or contact transmission for both dental practitioners and patients. Cheng et al. (2022)【2】highlighted that EOVs could be instrumental in reducing respiratory illness risks associated with prolonged exposure to contaminated air in clinical settings.
Challenges and Limitations
Despite their benefits, EOVs are not without challenges. First, their effectiveness is contingent upon correct placement and operational efficiency, which may vary across devices and clinical setups. Second, some practitioners report issues related to noise levels and patient comfort, which could affect compliance and workflow. Moreover, cost considerations may hinder widespread adoption, especially in resource-limited settings【4】.
Future Directions
Design Optimization
To enhance usability and efficacy, future iterations of EOVs should focus on ergonomic designs, noise reduction, and improved filtration systems. Integration with chair-side units and digital monitoring systems could also streamline their use in dental practices.
Broader Applications
While EOVs are predominantly used in dentistry, their application could extend to other medical disciplines involving aerosol-generating procedures, such as otolaryngology and respiratory therapy. Investigating cross-disciplinary use could expand their impact on infection control.
Longitudinal Studies
Further research is required to evaluate the long-term effectiveness and cost-benefit ratio of EOVs in clinical settings. Such studies would provide robust data to inform evidence-based guidelines for their implementation.
Conclusion
Extraoral vacuums offer a promising adjunct to conventional infection control measures, particularly in environments with high aerosol exposure. By capturing and neutralizing aerosols at the source, EOVs enhance safety for both practitioners and patients. However, addressing challenges related to device optimization, cost, and usability will be critical to maximizing their potential. With continued research and development, EOVs could become a standard component of infection control protocols in various medical fields.
References
- Gopalakrishnan, R., et al. Evaluation of extraoral vacuum devices in reducing aerosol dispersion during dental procedures. Journal of Dentistry and Oral Hygiene, 2021. DOI:10.34172/joddd.2021.033
- Cheng, L., et al. Extraoral vacuum systems as a mitigation tool for aerosol reduction in clinical settings. Journal of Endodontics, 2022. DOI:10.1016/j.joen.2022.09.007
- Hashimoto, T., et al. Effectiveness of bioaerosol capture by extraoral suction systems. Oral Medicine and Pathology, 2022. DOI:10.1002/1348-9585.12412
- Kimura, Y., et al. Aerosol management in dentistry: Evaluating the role of extraoral suction devices. Dentistry Journal, 2021. DOI:10.3390/dj9070080
Other related resources:
- Efficacy of extraoral suction devices in aerosol and splatter reduction during ultrasonic scaling: A laboratory investigation https://doi.org/10.34172/joddd.2021.033
- Clinical Efficacy of an Extraoral Dental Evacuation Device in Aerosol Elimination During Endodontic Access Preparation https://doi.org/10.1016/j.joen.2022.09.007
- Effective use of an extraoral vacuum in preventing the dispersal of particulate matter from metal dental materials https://doi.org/10.1002/1348-9585.12412
- Effects of Extraoral Suction on Droplets and Aerosols for Infection Control Practices https://doi.org/10.3390/dj9070080